The Integrated Cancer Research Core (ICRC) at The University of Texas Rio Grande Valley’s new, state-of-the-art McAllen Biomedical Research Facility is an investment in UTHealth RGV’s developing role in fast-tracking cancer research in the Valley and across Texas. As the only specialized facility of its kind within 250 miles, the ICRC enhances the university’s ability to foster the next generation of cancer researchers from the region.
The medically underserved Rio Grande Valley represents a hotspot of liver, gall bladder, stomach and cervical cancers. To address cancer disparities in this region, UTRGV received a $2.5 million CPRIT Core Facility Support Award (RP210180) in 2021 to create the ICRC.
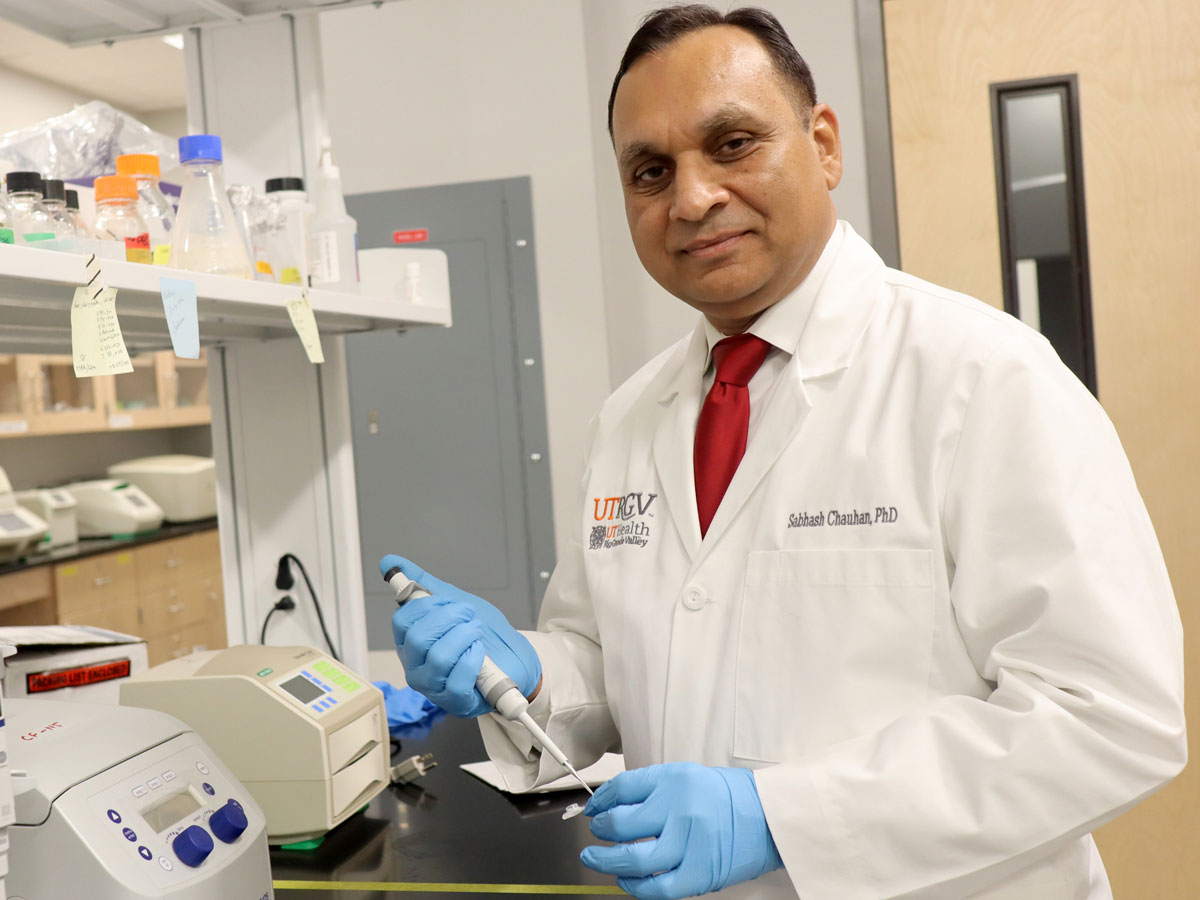
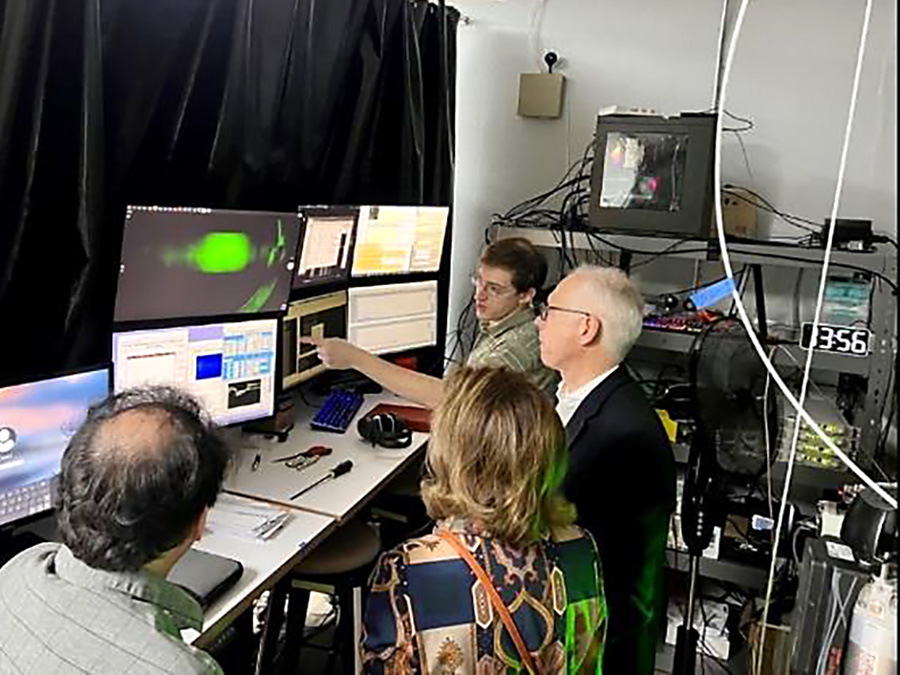
Directed by Subhash C. Chauhan, Ph.D., the ICRC provides cutting-edge technologies such as Flow Cytometry, CyTOF, Image Stream Flow, Droplet Digital PCR, and small animal imaging to support cancer research. Cost-effective access to modern research facilities in the region allows cancer investigators to work with local patient’s samples; facilitates new collaborative basic, translational, and clinical projects; and increases training opportunities for local medical personnel, undergraduate students, and medical residents in the RGV.
CPRIT awarded a $2 million First-Time, Tenure-Track CPRIT Scholar award (RR220081) to recruit Jonathan Clinger, Ph.D., from Cornell University to the Department of Chemistry and Biochemistry at Baylor University in Waco.
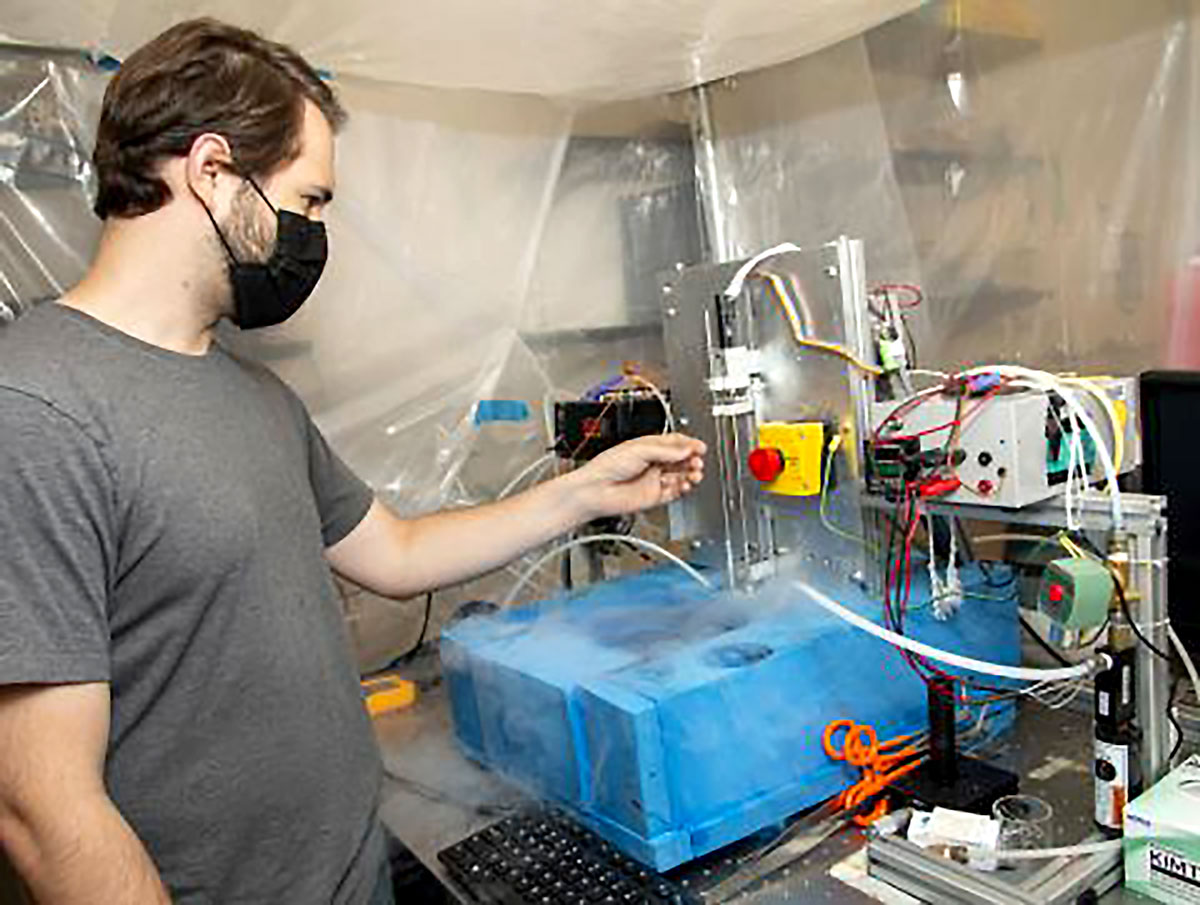
At Dr. Clinger’s lab, Baylor researchers study the structure and dynamics of proteins to better understand how proteins perform the physical and chemical jobs they do in living cells. Clarifying the 3-D structure of normal and altered proteins is essential for developing new cancer-fighting drugs but observing how the protein moves and changes shape while it is performing reactions is notoriously difficult. Dr. Clinger has devoted much of his career to developing new techniques – including a novel approach called Millisecond “Mix and Quench” – to observe these reactions more easily.
With the help of his CPRIT recruitment grant, Dr. Clinger is developing and commercializing his technique for broader applicability, including focusing on cancer relevant enzymes in the polyamine synthesis pathway, with the goal of improving the design of inhibitors by providing a superior structural starting point.
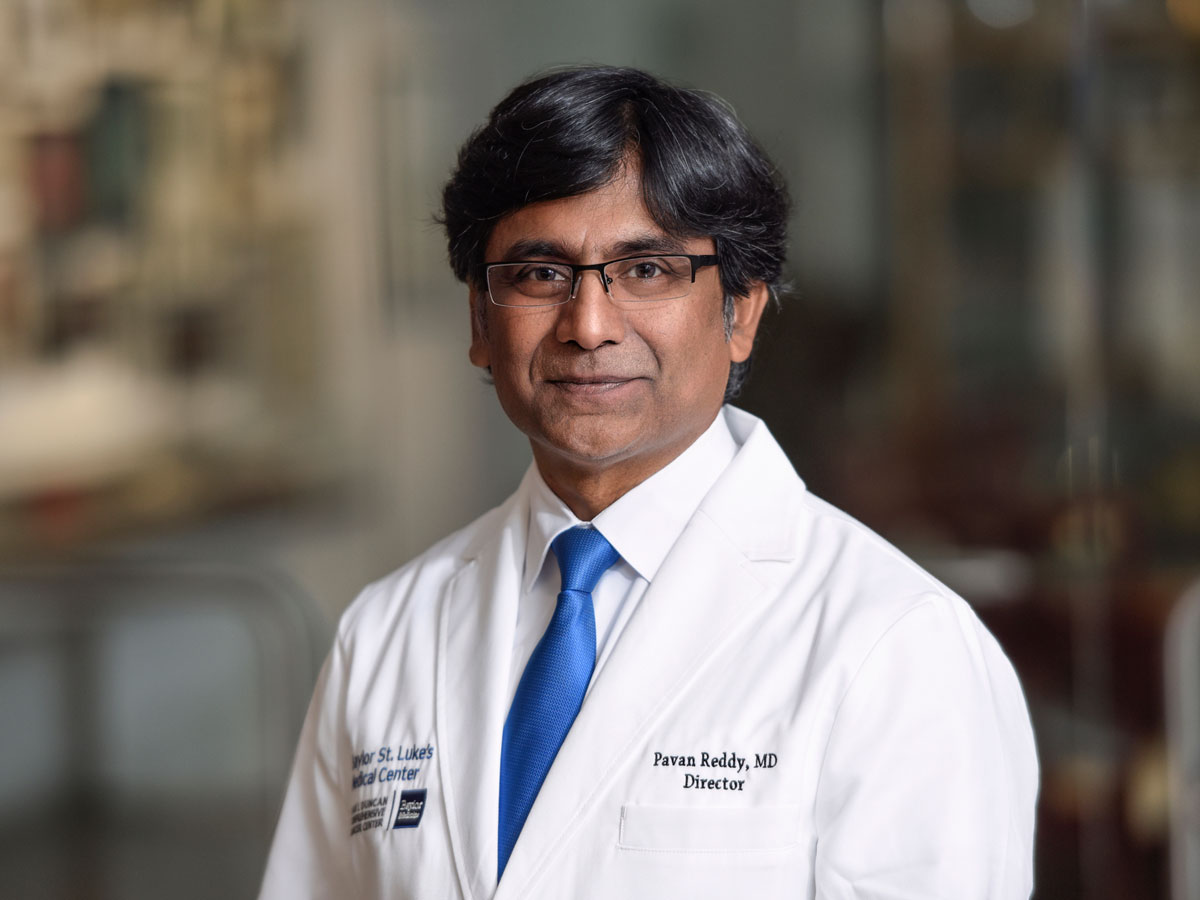
CPRIT works to build Texas’ cancer research capabilities along the entire academic spectrum, from early investigators to nationally recognized leaders in the field. Baylor College of Medicine in Houston was awarded a CPRIT Scholar grant (RR220033) to to bring Pavan Reddy, M.D., a renowned physician-scientist and leader in the field of cell therapy and stem cell transplantation, to Texas. Formerly Deputy Director of the University of Michigan Rogel Cancer Center, Baylor College of Medicine named Dr. Reddy Director of the Dan L. Duncan Comprehensive Cancer Center following the CPRIT award.
Dr. Reddy specializes in hematological malignancies, with research experience spanning basic immunology to translational proof-of-concept clinical trials. He has a recognized ability to translate insights from his laboratory observations to clinical testing in patients with blood cancers undergoing stem cell transplantation. Dr. Reddy has a stellar track record, with over 200 published original research articles and support from the National Institutes of Health, the Leukemia and Lymphoma Society, the National Marrow Donor Program and the American Society of Transplantation.
At Baylor College of Medicine, Dr. Reddy is extending his earlier work to overcome the factors that limit the curative potential of T-cell immunotherapy and therapy with immune checkpoint inhibitors. Dr. Reddy reinforces the stature of the Duncan Center as an academic powerhouse of innovation and transformative cancer care.

No one is safe from cancer, regardless of their gender, ethnicity or income; however, the burden is greater for certain populations based on their socioeconomic status, racial/ethnic group, and cancer type. Cancer is the leading cause of death among Hispanics, yet Hispanic cancer patients are underrepresented in cancer research.
With its Center for the Study of Hispanic Cancer Disparities, The University of Texas at El Paso (UTEP) is a hub for biomedical research that addresses health issues affecting the Hispanic community. CPRIT awarded a $5.8 million Texas Regional Excellence in Cancer (TREC) Award (RP210153) to UTEP in 2021 to support excellence in multidisciplinary, culturally relevant research, and cancer prevention to increase health equity throughout the region. This program will create a core group of well-trained, independently funded scientists equipped to lead interdisciplinary team-based grant projects and tackle some of the border region’s most pressing health issues, and mentor future generations of cancer disparities researchers.
Led by UTEP’s Marc Cox, Ph.D., MSPH, the program trains early-stage investigators, hires additional researchers with a strong background in cancer disparities research, and provides professional development opportunities to enhance researcher’s success and impact in the area of Hispanic cancer disparities. Additionally, established investigators at The University of Texas MD Anderson Cancer Center mentor each UTEP researcher.

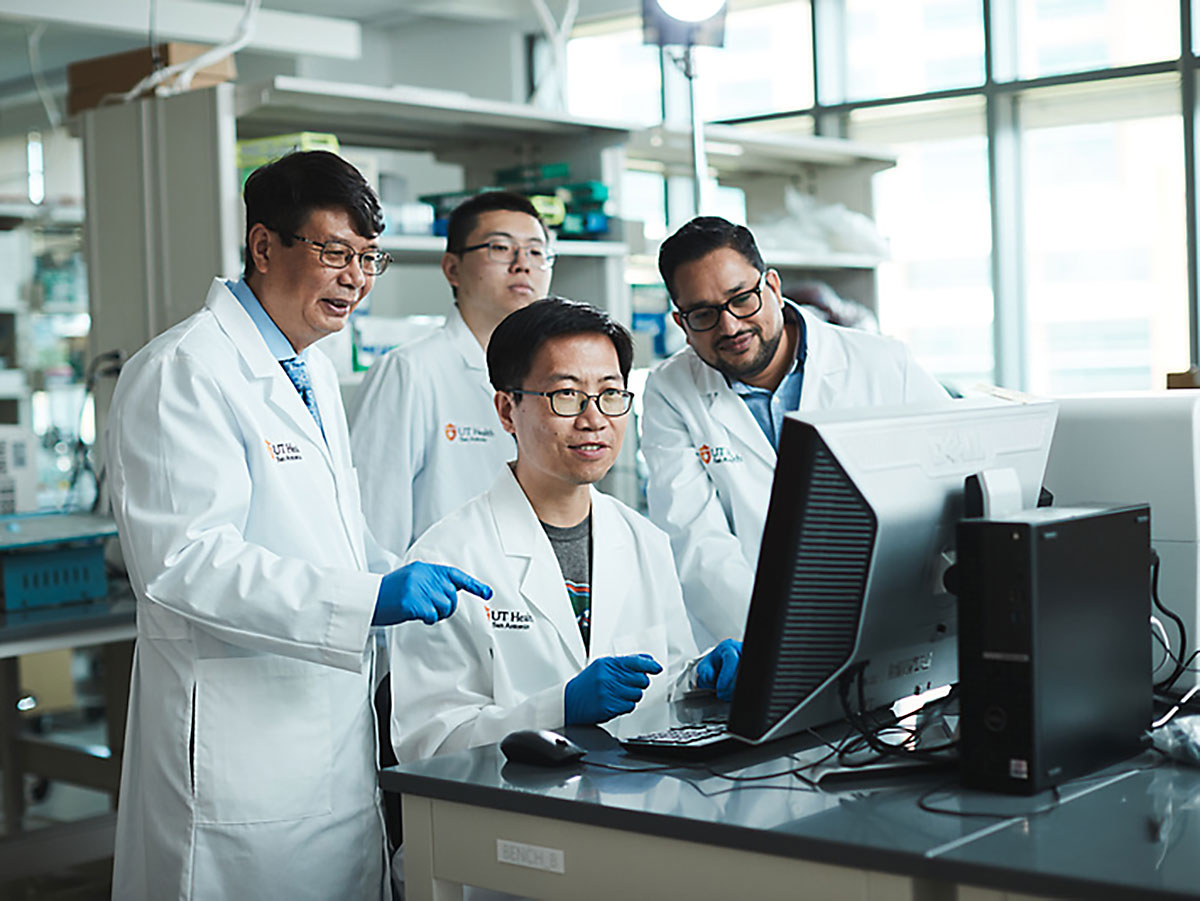
In another example of CPRIT’s top level impact in cancer research, The University of Texas Health Science Center at San Antonio recently recruited world-renowned researcher Reuben Harris, Ph.D., from the University of Minnesota, with the support of a five-year, $6 million Recruitment of Established Investigators grant (RR220053). At UT Health San Antonio, Dr. Harris serves as the Chair in the Department of Biochemistry and Structural Biology. In addition to the many awards and recognition in his distinguished career, he has been a Howard Hughes Medical Institute Investigator since 2015, a position that transferred with his recruitment, making him the first HHMI Investigator at UT Health San Antonio.
Dr. Harris runs an internationally renowned research program explaining mechanisms of DNA mutagenesis in cancer and pathways of tumor evolution, and the discovery and development of novel cancer therapeutics. He pioneered a new area of mutagenesis research with his discovery of a novel function for the APOBEC family of RNA-modifying enzymes. APOBEC-mediated DNA deamination dominates the mutational landscape of many tumors, playing a pivotal role in tumor initiation and progression. Dr. Harris will extend this work to uncover novel synthetic lethal interactions (a cellular state whereby the combination of deficiencies of two or more proteins leads to cell death) that researchers can develop into new therapies for APOBEC-positive tumors.

In the U.S., cervical cancer incidence and mortality rates have decreased by 70% due to improvements in screening and testing programs, as well as uptake and efficacy of HPV vaccines. However, medically underserved areas like the Lower Rio Grande Valley (LRGV), where the vaccination rates remain lower than the US overall, have not seen the same success due to a lack of access to screening programs and insufficient availability of local providers. Cervical cancer mortality is approximately 30% higher in the LRGV compared with non-border Texas counties.
Since 2014, CPRIT has awarded three prevention grants totaling more than $6 million (PP150012, PP190014 & PP220037) to fund a cervical cancer prevention program that combines public education, local provider training, screening services, and patient navigation. The program, directed by Kathleen M. Schmeler, M.D., at The University of Texas MD Anderson Cancer Center, has educated more than 10,000 women in medically underserved counties across Texas, including the Rio Grande Valley about the importance of cervical cancer screenings.
With CPRIT support, Dr. Schmeler’s program cultivates the life science infrastructure in these communities by using remote learning to train local providers to evaluate and manage abnormal cervical cancer screening tests. As a result, providers have screened almost 20,000 women and diagnosed and treated over 1,035 women for cervical dysplasia and cervical cancer.

A key component of bolstering the life science infrastructure in Texas is training the next generation of researchers. To expedite cancer research innovation and prevention, CPRIT supports programs that train students to challenge and break out of current research and practice paradigms. One such program is the Innovation in Cancer Prevention Research Training Program at The University of Texas Health Science Center at Houston. Since 2014, CPRIT has partnered with UT Health Houston to train outstanding doctoral students and postdoctoral fellows from diverse disciplines who are committed to a career in cancer prevention research and eliminating health disparities.
One of the program’s many successes include Jane R. Montealegre, M.D., who completed her training in 2013 and is now assistant professor and Deputy Director of Outreach and Health Disparities at the Dan L Duncan Comprehensive Cancer Center at Baylor College of Medicine. Dr. Montealegre is an expert in health disparities and preventive healthcare utilization among immigrants, racial/ethnic minorities, and the medically underserved and has received three CPRIT prevention grants (RP140103, RP160015 & RP210042) totaling $6.2 million to work with safety net health systems to increase HPV vaccinations and tobacco cessation efforts.
CPRIT’s success in expanding the life science infrastructure in Texas is evident in the partnerships fostered by CPRIT funding.
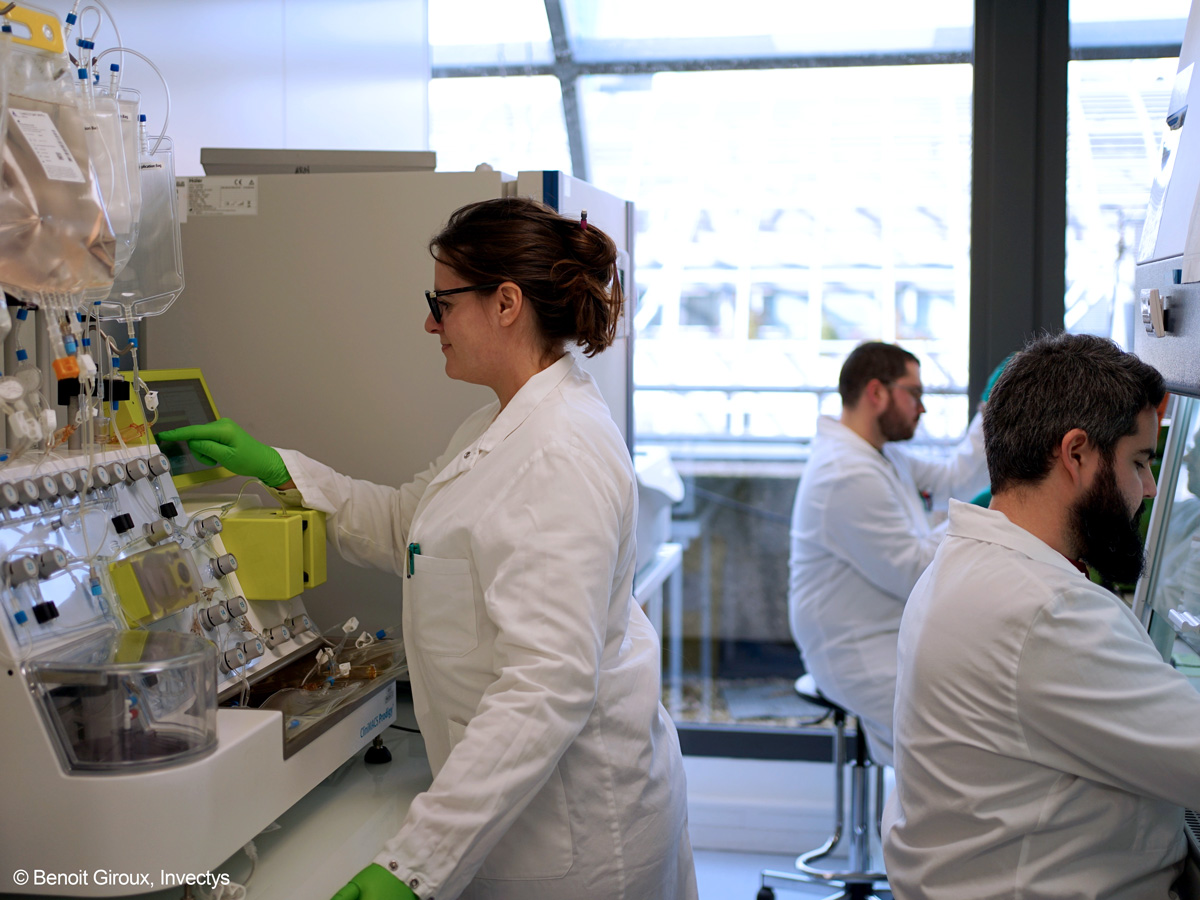
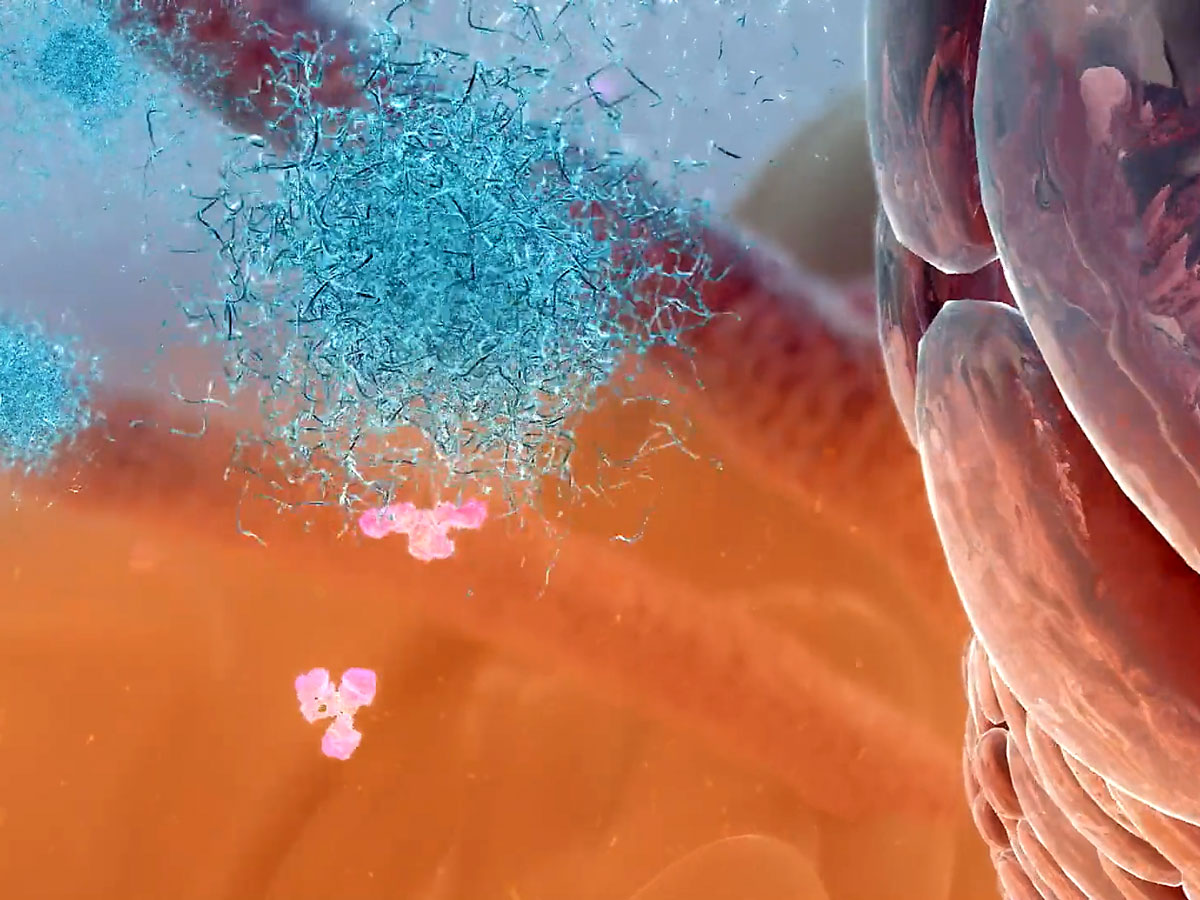
In 2020, CPRIT awarded a Company Relocation Product Development Research Award totaling $14,196,990 (DP200034) to Invectys USA, Inc., a biopharmaceutical company developing innovative anti-cancer products in immunotherapy based on leading technology from the world-renowned Pasteur Institute in Paris. The company chose Houston as their U.S. location to advance its novel chimeric antigen receptor (CAR) T platform and to conduct early-stage clinical studies. Invectys’ research focuses on the HLA-G molecule, a powerful modulator of the human immune system that normally protects a fetus during pregnancy. However, HLA-G is in cancer cells, suppressing a patient’s own body’s immune response to the disease. Invectys’ technology is designed to target and remove tumor cells that express HLA-G, thus reducing these immunosuppressive effects and thereby reactivating the patient’s own immune system. Mice treated with anti-HLA-G CAR-T cells have shown a near-total absence of tumor growth.
Additionally, The University of Texas MD Anderson Cancer Center recently announced a collaboration with Invectys and the Cell Therapy Manufacturing Center (CTMC) to advance these new CAR-T cell therapies through preclinical development into early-phase clinical studies. The collaboration links the clinical trials expertise of MD Anderson with the technology created by Invectys and the cell therapy expertise of CTMC.
This kind of cross-collaboration spurred by CPRIT funding is bringing together the finest Texas has to offer in fighting cancer.
Lutetium-177 (177Lu) is a radioisotope approved for use in treatments for certain neuro-endocrine cancers as well as prostate cancer, the second leading cause of cancer death in men. While cancer therapies based on this radioisotope are proving highly effective, the world supply of the stable Ytterbium-176 (176Yb) isotope needed to make 177Lu is limited and endangered. 176Yb is currently only available in small quantities - measured in grams per year - from Russia, a geopolitically unstable source. Scientists need a reliable, domestic source of pure 176Yb to produce sufficient 177Lu to support FDA-approved drugs and ongoing cancer research, trials, and therapies in Texas and around the globe.
CPRIT awarded a $2.5 million Texas Company Product Development Research Award (DP220055) in 2022 to Atom Mines. The Austin-based company utilizes an isotope separation technology to enable domestic production of Ytterbium-176 in sufficient quantities that meets the quality criteria for isotope purity. Developed by Mark G. Raizen, Ph.D., professor at The University of Texas at Austin, the Magnetically Activated and Guided Isotope Separation (MAGIS) technology promises to overcome the 176Yb production bottleneck and will make Lutetium-177 available in large quantities to pharmaceutical companies worldwide to treat hundreds of thousands of patients each year.
Atom Mines will use CPRIT’s grant to increase the production of 176Yb. The company has already produced small quantities of medical grade (99.5%) 176Yb and secured a funded distribution partnership with Eckert & Ziegler.
CPRIT’s investment in Atom Mines will ensure greater access to these isotopes and put cancer treatment and medical research institutes in Texas at the forefront of these therapies.

Breast cancer is the most common type of cancer for women in Northeast Texas and the second most common cause of cancer deaths among women. CPRIT awarded a $1 million Evidence-Based Prevention Programs and Services grant (PP220035) to Paul McGaha, D.O., MPH, Department Chair of Preventive Medicine and Population Health at The University of Texas Health Science Center at Tyler (UTHSC Tyler) to partner with underserved East Texas communities to provide breast cancer screening services to detect the disease at earlier stages when it is easier to treat.
The DEFEAT (Delivering Education, Focused Navigation, and Equitable Access throughout East Texas) program focuses on recruiting underserved and uninsured women, between the ages of 40 to 75, for proper access to breast cancer screenings. Unlike other urban and suburban screening projects, the team developed a unique integrated public health and clinical model to optimize success in rural East Texas. This “access to care” model leverages the availability of primary care programs at UTHSC Tyler and incorporates strong partnerships with community health facilities to create awareness of breast cancer screening options and to recruit screening participants.
This CPRIT grant will educate 6,000 individuals and 600 professionals and provide breast cancer screenings to 1,220 patients.
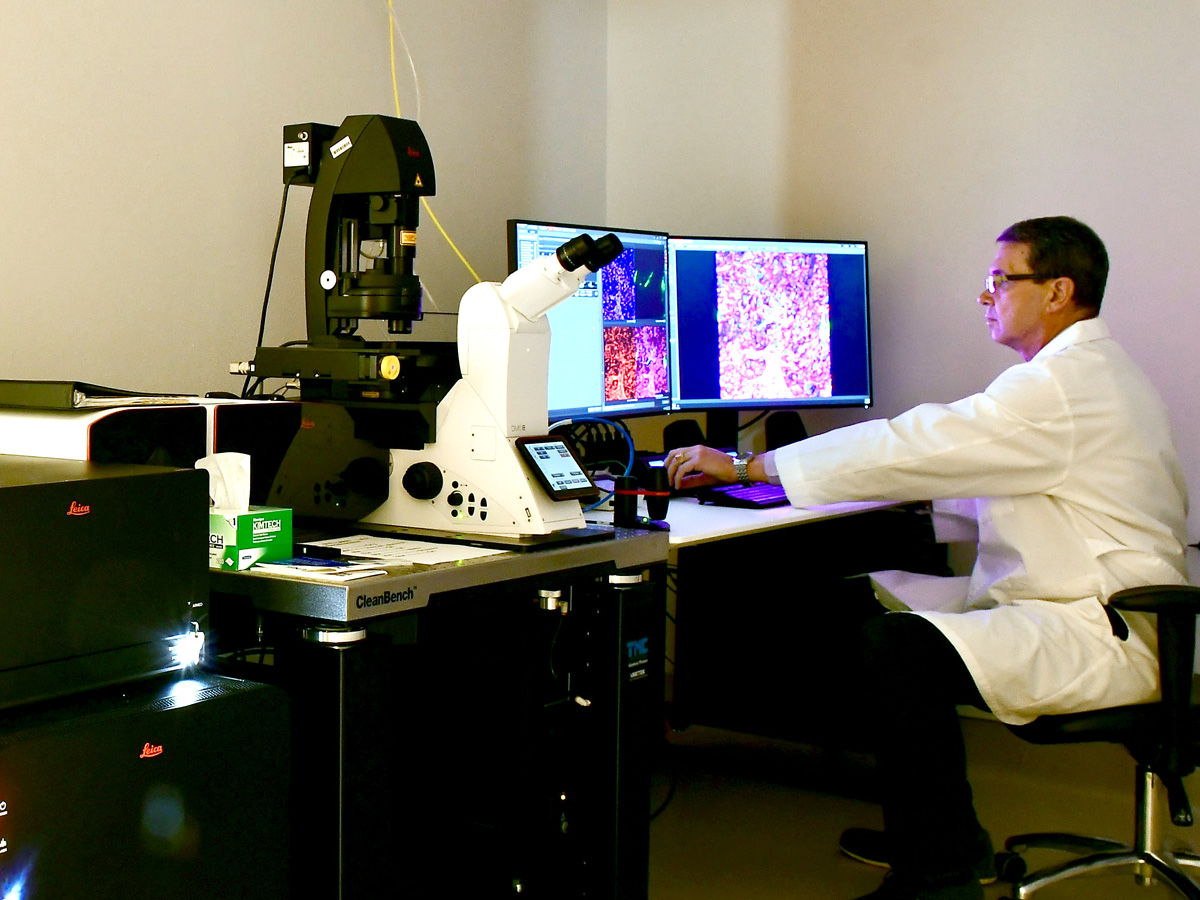
A state-of-the-art imaging facility is an indispensable component of biomedical research. To support research growth and advance cancer fighting goals at Texas Tech University Health Sciences Center (TTUHSC) in Amarillo, CPRIT awarded a $2.8 million Core Facilities Support Award (RP200572) to the Jerry H. Hodge School of Pharmacy to expand researchers’ cell imaging capabilities.
Imaging Core Facility lab instruments funded through this grant allow greater optical imaging of living cells and will greatly enhance the quality of obtainable data in cancer research projects. One specialized instrument is the IR VIVO, an infrared multispectral imager also used for small animal studies in partnership with the Texas Tech School of Veterinary Medicine. IR VIVO takes advantage of the most recent developments in shortwave infrared imaging with an ultra-low-noise InGaAs camera, novel homogeneous illumination, and powerful analytical software to provide an unprecedented combination of fast, high resolution and deep imaging.
With CPRIT’s grant and the new capabilities of the Imaging Core Facility, led by Ulrich Bickel, M.D., TTUHSC and West Texas researchers are expanding their insight into the science of medicine, and driving forward advancements in cancer treatments, prevention, and cures.
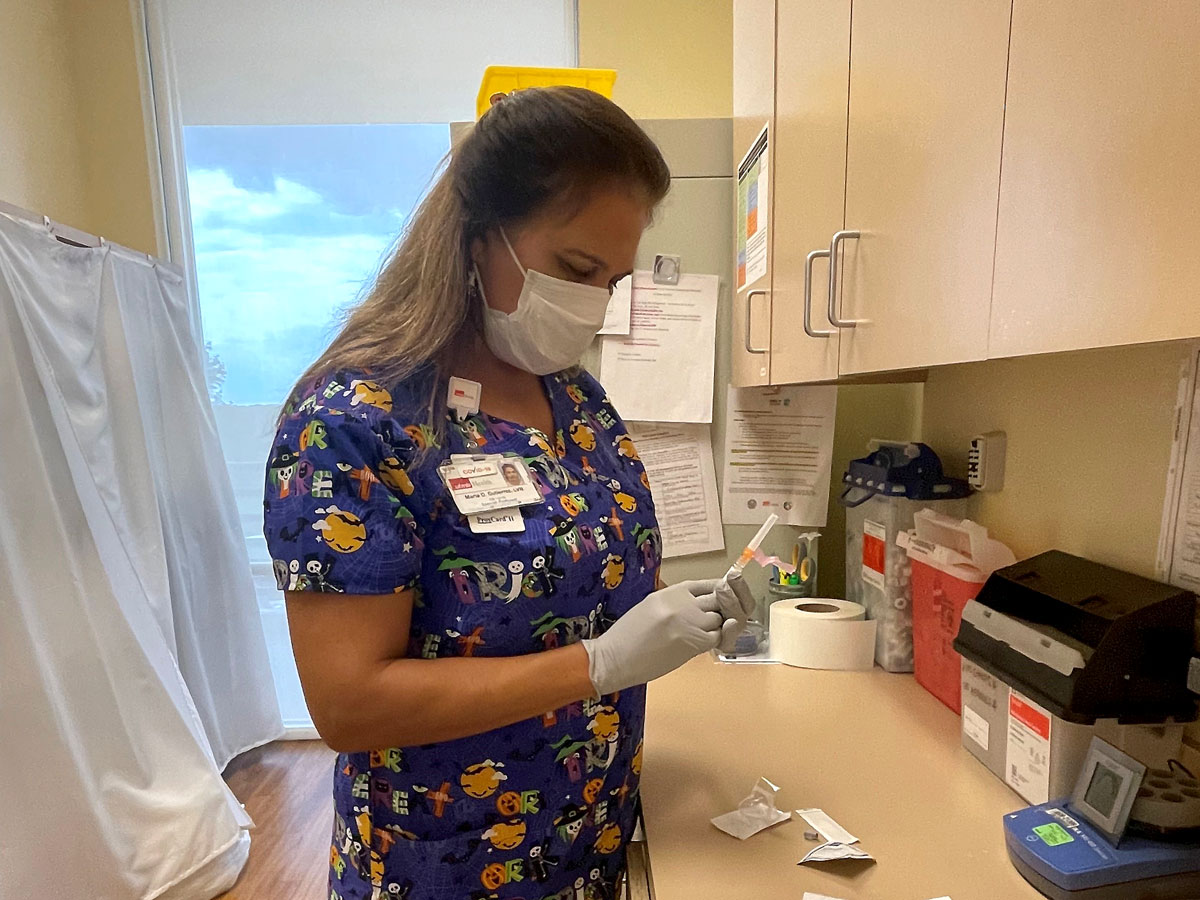
Over the last decade, CPRIT has awarded 10 grants totaling over $17.6 million to support the human papillomavirus (HPV) vaccination efforts of Abbey Berenson M.D., Ph.D., at The University of Texas Medical Branch Galveston (UTMB).
Dr. Berenson is a senior clinical researcher, gynecologist, professor, and mentor, with an international reputation for studies of health issues among reproductive-aged women. She is tireless in her work to increase HPV awareness and vaccination rates among young women (< 26 years of age) living in southeast Texas, including the Rio Grande Valley. CPRIT funding of Dr. Berenson’s work at UTMB enabled HPV vaccination of over 1,500 uninsured women who otherwise would not have gotten vaccinated due to cost and enabled the education of hundreds of health care professionals in UTMB clinics in Galveston and Hidalgo County on HPV and vaccination guidelines.
Also, Dr. Berenson trains the next generation of early career investigators from an array of medical disciplines, the majority of whom have remained in academic research and have obtained funding as principal investigators on their own external awards.
In August 2021, the American College of Obstetrics and Gynecology recognized Dr. Berenson as a 2021 Immunization Champion for her exceptional progress in increasing immunization rates among adults and pregnant women in their communities through leadership, innovation, collaboration, and educational activities.

The best hope for surviving cancer, regardless of socioeconomic or regional barriers, is finding the cancer early. The Breast Cancer Education Screening and NavigaTion (BEST) project at Texas Tech University Health Sciences Center in El Paso provides cancer education and no-cost screening and diagnostic testing to uninsured/underinsured Hispanic women in over 100 West Texas counties, including El Paso and Hudspeth counties.
The BEST project is a culturally tailored, comprehensive multicomponent intervention that uses a socioecological approach to address known barriers to breast cancer screening, diagnosis and treatment.
CPRIT has awarded the BEST project three grants (PP180003, PP210004 & PP130068) totaling more than $5 million since 2013. Through the BEST program, Jennifer Molokwu, M.D., MPH, and Pracheta Matharasi, MPH, have created a cancer prevention network throughout the region comprised of over 200 organizations including clinics, hospitals, radiology service providers, and a multitude of community-serving organizations. The most recent CPRIT grant will help expand access to additional rural and medically underserved West and South Texas counties, and integrate novel outreach, education and navigation approaches to maximize program impact.
One of the most prominent ways CPRIT funds innovation in cancer treatments and cures is through our Product Development Research Program. CPRIT provided almost $18 million in two grants (DP200018, DP210005) to Dialectic Therapeutics, a Dallas biotech start-up dedicated to the development of impactful and exceptional drugs to treat cancers when there are few to no other options.
Dialectic’s lead candidate is DT2216, is a novel Antiapoptotic Protein Targeted Degradation (APTaD™) compound that causes B-cell lymphoma cells to degrade, thereby becoming more susceptible to chemotherapy. Preclinical studies show that DT2216 is highly effective because cancer cells are less likely to develop resistance to this compound compared to other chemotherapy drugs.
CPRIT supported Dialectic’s preclinical efforts with a Seed Award for Product Development Research in 2020, followed by a CPRIT Texas Company Product Development Research grant for continued clinical development of DT2216 in 2021. Robert Hromas, M.D., Dean of the Long School of Medicine at The University of Texas Health Science Center San Antonio and Daohong Zhou, M.D., Co-Director of the Center for the CPRIT-funded Center for Innovative Drug Discovery (CIDD) were scientific co-founders of Dialectic.
In 2022, DT2216 received Orphan Drug Designation and Fast Track Designation from the FDA for the treatment of T-cell lymphoma. Dialectic has announced their first-in-human dose in a Phase 1 clinical trial evaluating DT2216.
With CPRIT’s help, Dialectic hopes DT2216 will provide cancer patients who have little hope with increased disease-free survival.
The CPRIT Product Development Research Program funds the commercial development of novel products that offer therapeutic or diagnostic benefits not currently available. These product development investments also stimulate the life sciences ecosystem in Texas and provide long-term returns for Texans suffering from the burden of cancer.

OncoNano Medicine is a clinical stage biopharmaceutical company specializing in innovative prevention and treatment of cancer. OncoNano’s proprietary product candidates include solid tumor therapeutics, agents for real-time image-guided surgery, and T cell activating immunotherapies. CPRIT has supported the development of OncoNano’s product candidates, ONM-501 and Pegsitacianine intraoperative imaging agent, with three Product Development Research grants (DP200081, DP140072 & DP190066) totaling $31.4 million.
Chief Medical Officer Kartik Krishnan, M.D., Ph.D., explained that OncoNano’s OMNI™ platform is composed of proprietary polymers tailored to activate Stimulator of Interferon Genes (STING), part of the body’s host defense system against viruses. STING activates both the T cell and the innate immune response against solid tumors. The lead imaging agent, Pegsitacianine, is a fluorescence-based IV injectable used to guide surgeons in the detection of cancerous tissue in patients while undergoing removal of their solid tumor.
Phase 1 and on-going Phase 2 trials have shown that Pegsitacianine detects many solid cancers, has a favorable safety profile, and provides evidence of tumor-positive margins or hidden disease detection that was missed by standard-of-care detection methods.

Survivors of childhood cancer face many health challenges as they age. Because of their exposure to chemotherapy, radiation, surgery, or other treatments, these survivors, many now well into adulthood, experience late effects or health problems directly related to their cancer treatment. Creating a long-term care program for these survivors is vital. However, many childhood cancer survivors, especially those in underserved areas, lack access to continued medical care.
To address this important public health problem, CPRIT supported the creation of the “Passport for Care” (PFC) program at Baylor College of Medicine. Passport for Care is an online interactive free resource for clinicians and childhood cancer survivors that provides patients and survivors of chronic illnesses with increased access to their medical information, including survivorship care plans. Created in 2010 with a CPRIT prevention grant (PP100090), PFC has received three expansion grants for a total of almost $5 million in funding. Since its inception, hospitals and clinics worldwide have adopted the PFC model, enrolling over 45,000 survivors to date.
Maria Gramatges, M.D., Ph.D., and her team will use the most recent CPRIT grant (PP220017) to establish a bilingual survivorship education program at the Vannie E. Cook Jr. Cancer and Hematology Clinic in McAllen, the only pediatric cancer treatment facility serving the Rio Grande Valley. Using bilingual Survivorship Navigators and evidence-based screening and follow-ups, Dr. Gramatges hopes to overcome barriers to clinical service delivery with innovative, sustainable solutions that lead to improved outcomes for childhood cancer survivors in the RGV.

Computational biology involves the analysis and discovery of biological phenomena using computational tools, and the algorithmic design and analysis of such tools. CPRIT’s Oversight Committee approved computational biology as a CPRIT Academic Research program funding priority because of its significant potential to advance cancer research.
The University of Texas at Austin received a $1.2 million CPRIT Individual Investigator Research Award (RP220225) in 2022 to fund a project led by David Hormuth, Ph.D., to integrate predictive mathematical models with patient-specific data to help guide cancer care.
Dr. Hormuth, a biomedical engineer at UT Austin’s Oden Institute for Computational Engineering and Sciences, is developing a clinical-computational framework to predict and spatially-map more aggressive and treatment-resistant tumor regions that will enable personalized treatment in patients receiving radiation therapy for gliomas. His project integrates multiparametric magnetic resonance imaging data with mechanism-based mathematical modeling to predict disease response.
The ability to predict spatiotemporal disease progression is a paradigm shift in glioma treatment. Clinicians will use these individualized tumor “forecasts” to select and adapt treatment in real time to optimize the ability to target resistant disease, rather than waiting to see if the tumor grows post-treatment.

Baylor College of Medicine brought Anthony M. Mustoe, Ph.D., to Texas from the University of North Carolina, Chapel Hill with a $2 million CPRIT Scholar grant (RR190054) in 2019 to study the role of RNA in the initiation and promotion of cancer. His primary focus is to develop new chemical and computational methods that enable high-throughput quantitative measurement of RNA structure and dynamics inside of living cells. Knowledge of RNA structure in turn provides a foundation for defining biophysical mechanisms of RNA regulation.
Dr. Mustoe’s lab focuses on the basic understanding of cancer mechanisms, with its research findings applicable to many different types of cancers. Maximizing the impact of CPRIT’s investment, Dr. Mustoe also dedicates time to collaboration and interdisciplinary science and provides a supportive environment for young scientists to gain integrated training at the interface of experiment and computation.
“One of the hopes of RNA therapeutics is the potential for custom drugs that precisely target patient-specific mutations,” Dr. Mustoe explains. “This level of customization is just frankly impossible in the traditional route of targeting proteins.” He credits CPRIT funding for allowing him to tackle “big risky questions that I normally wouldn’t feel comfortable or able to tackle because those resources allow me to make big bets, with the understanding that some of them may not work out but with the hope that a few of them will.”